New advanced technology to help you recover quicker.
An in depth look at how it works.
Getting strong is hard. Rehab after injury is hard. Unfortunately, losing muscle after periods of inactivity or immobilization is not hard. Muscle is easy to lose, but hard to gain. Even brief periods of decreased activity can cause a significant amount of muscle loss — leading to weakness and a prolonged rehabilitation.
One of the most difficult parts of recovering from surgery or an injury, is gaining back the muscle you lost. It’s hard work and it takes a lot of time. What if we could prevent you from losing muscle in the first place? Recovery would be quicker and you’d be better off in the long run.
Good news! Impact Rehab & Wellness now offers Blood Flow Restriction Rehabilitation, which does just that!
What is Blood Flow Restriction Training?
Blood flow restriction (BFR) is the brief and intermittent occlusion of venous blood flow, using a tourniquet, while exercising. The goal is to reduce enough blood flow to create the desired effect. This is performed via a specialized tourniquet system with a built-in monitor, which maintains the desired limb occlusion pressure.
In cases where strength or hypertrophy (growth) is needed, blood flow restriction can be utilized. BFR stimulates muscle hypertrophy by increasing muscle activation and muscle swelling. BFR training has been shown to increase muscle hypertrophy and strength at much lower intensity than traditional workouts. This makes it safer for injured tissues and joints.
Post Surgery/Injury Muscle Loss
We all know that going very long without moving causes weakness. Think about any time you’ve been sick and how weak you feel afterwards. That’s because it doesn’t take very long to begin losing muscle.
A study in the Journal of Physiology showed that 14 days of knee immobilization in otherwise healthy adults resulted in a 31% decrease in strength in the immobilized leg. Additionally, the participants lost 350 grams (approximately 3/4 lb) of quadriceps muscle.
Another study decreased the daily step count of elderly subjects by 76%. This resulted in measurable reduction in lean muscle mass and impaired insulin sensitivity in just 2 weeks.
Both studies found that it was a decrease in muscle protein synthesis that led to anabolic resistance — reduced stimulation of muscle protein/amino acids.
Ultimately, this means one of the biggest obstacles holding you back from a quick and efficient post-op rehabilitation is loss of muscle and strength.
Muscle Physiology
To really understand the benefits of BFR , it helps to have a basic understanding of muscle physiology. There are different types of muscle fibers in your body, which are classified based on how they produce energy. The different muscle fibers can be trained using specific exercises. These exercises are designed to focus on how they create energy or generate force. While a variety of types of muscle fibers have been identified, they’re generally classified as being either slow-twitch or fast-twitch.
Slow-Twitch Fibers
Slow-twitch fibers contain mitochondria, the organelles that use oxygen to help create adenosine triphosphate (ATP). ATP is the chemical that fuels muscle contractions. These fibers are considered aerobic. The tonic muscles, responsible for maintaining posture, have a high density of these fibers. Steady-state endurance training can help increase mitochondrial density, which improves the efficiency of how the body uses oxygen to produce ATP.
Slow-twitch fibers can sustain force for an extended period of time because they provide their own source of energy. However, they aren’t able to generate a significant amount of force. Due to their low activation threshold, they are the first recruited when a muscle contracts. If they can’t generate the amount of force necessary for the specific activity, the fast-twitch fibers are engaged.
Fast-Twitch Fibers
Fast-twitch fibers can be further classified into fast-twitch type IIa — fast oxidative glycolytic — and fast-twitch type IIb — fast glycolytic. Fast oxidative glycolytic type use oxygen to help convert glycogen into ATP, while fast glycolytic type rely on ATP stored in the muscle cells to generate energy.
Fast-twitch fibers have a high threshold and will be activated only when the force demands are greater than the slow-twitch fibers can meet. The larger fast-twitch fibers take a shorter time to reach peak force. They can generate higher amounts of force than slow-twitch fibers, but they’re quicker to fatigue. The phasic muscles, responsible for generating movement in the body, contain a high density of fast-twitch fibers.
Strength and power training can increase the number of fast-twitch muscle fibers recruited for a specific movement. Fast-twitch fibers are responsible for the size and definition of muscles.
Blood flow restriction targets the fast-twitch muscle fibers.
Nutrition
The Recommended Dietary Allowance (RDA) for protein is calculated based on the maintenance of these functions. That means you need 0.36 grams of protein per pound of body weight to stay alive and healthy. However, this is not nearly enough protein to build muscle.
In a review by Brad Shoenfeld and Alan Aragon, the authors conclude that daily protein intake of 1.6 – 2.2 grams of protein per kilogram of body weight maximizes muscle building. That is 0.72 – 1 gram per pound of body weight. This amount should reduce anabolic resistance and allow for regaining of lost muscle, as long as there’s enough stimulus provided to gain muscle.
Anabolic resistance contributes to declines in skeletal muscle mass. In other words, if your body doesn’t have enough protein to feed your muscles, it will begin cannibalizing the muscles. Therefore, it’s vital to make sure you’re getting enough protein, especially if you’re trying to build muscle.
Muscle Growth
The American College of Sports Medicine suggests that to gain strength and hypertrophy, you need to work out at 60-85% of your 1 repetition maximum (RM). You do this for 3 sets of 8-12 reps and you need to lift 2-3 days per week. This can be difficult, or impossible, if you’re recovering from a soft tissue or joint injury.
Tissue load refers to any internal or external force produced on a muscle at any given time. Load can be expressed via total training volume, load intensity, load frequency, and load type (maximal, dynamic, repetitive).
Muscle hypertrophy usually occurs from an overload stimulus. This is done by progressively increasing an external load using at least 70% of your 1RM for a specific lift. This intensity of load is known as High Intensity Training (HIT). HIT is defined as using a resistance between 65-90% of 1RM. Hypertrophy is thought to occur by muscle tension, muscle damage, and metabolic stress.
Muscle Tension
Mechanically induced tension through the muscle during weight training is an essential component of the adaptive response. Simply put, providing the muscle with mechanical overload produces muscle mass. However, muscle tension is not the sole reason for hypertrophy adaptations. Extremely high loads may promote neural adaptations, not necessarily structural ones. Therefore, higher loads don’t always equate to higher hypertrophy levels.
Muscle Damage
The feeling of soreness in the days after training is due to localized damage and disturbance. It’s a typical response to weight training and has been likened (on a cellular level) to that of the acute phase inflammatory response. This process has been linked to a number of growth responses that play a role in adaptation.
Metabolic Stress
Weight training assists in the production of a number of metabolic by-products that have been theorized to signal a process of cell swelling as a method of self-preservation and protection. The cell adapts by becoming stronger and increasing its integrity — again, a method of adaptation. However, for many people this type of HIT is not possible due to illness or injury.
A typical alternative approach is using low resistance, like elastic bands, to start loading the tissue. Unfortunately, a low load on tissue cannot improve strength or hypertrophy. Motor unit recruitment is the major benefit of low load training. This is a measure of how many motor neurons are activated in a particular muscle and, therefore, how many muscle fibers are activated. The higher the recruitment, the stronger the muscle contraction will be.
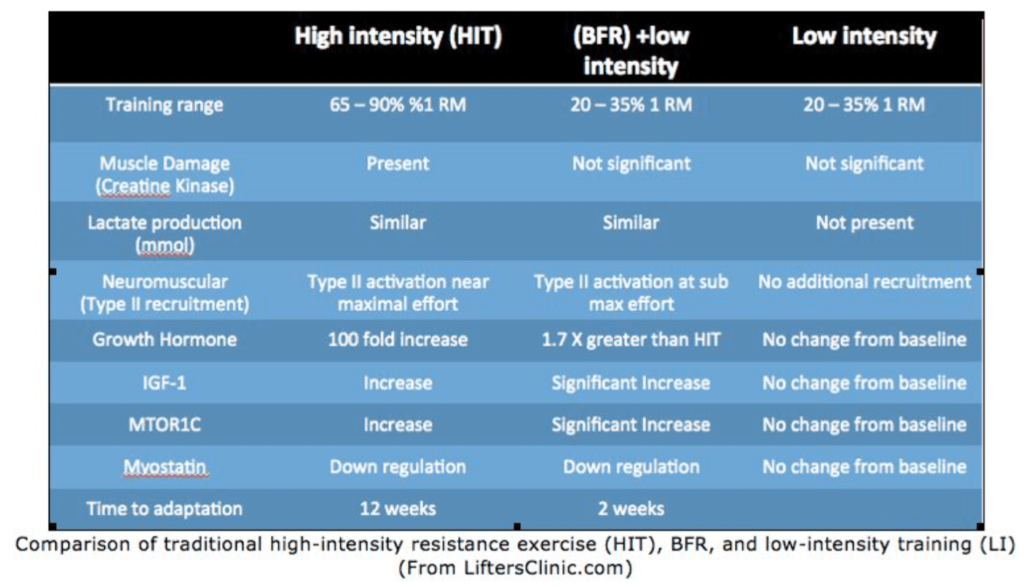
How Does BFR Compare to Traditional Strength Training?
Compared to standard weight training, BFR stimulates muscle growth and strength in about half the time and using 1/3 of the weight. By reducing venous return, BFR forces blood to remain inside your extremities longer than usual. The blood remaining in the muscle leads to faster muscle fatigue and muscle failure, which stimulates faster repair and regeneration. This results in rapid muscle strength and growth.
BFR combined with low intensity resistance exercise (20 – 30% 1 rep. max) has been observed to result in significant skeletal hypertrophy and strength within as little as 2 weeks. Additionally, minimal time allowance is necessary to see benefits. In comparison, traditional resistance training recommends lifting loads greater than 65% of a 1 rep. max (1 RM) over a period of 6-12 weeks to get strength and hypertrophy gains.
BFR stimulates muscle hypertrophy by increasing muscle activation and muscle swelling. Similar to a rehabilitation schedule, low intensity training combined with BFR training only 2-3 days per week resulted in the greatest effect size compared to training 4-5 days per week.
A study published in the Journal of Strength and Conditioning Research investigated the acute effects of low intensity, practical BFR on muscle activation, swelling, and damage. The study found that practical BFR significantly increased muscle activation, as well as muscle thickness, without increasing indications of damage to the muscles. Therefore, BFR enables you to get a high intensity workout with minimal risk while using very light weights at high repetitions.
Traditional physical/occupational therapy uses low resistance techniques. While this helps with range of motion and neuromuscular re-education, it doesn’t increase strength. By integrating BFR into rehab, we can build muscle strength safely and effectively.
– Michael Siegenthaler, PT, DPT
If you are interested in learning more about BFR or checking to see if you’d benefit from BFR as part of your treatment plan, please use our interest form below:
References
Abe, T., et al. “Skeletal Muscle Size and Circulating IGF-1 Are Increased after Two Weeks of Twice Daily ‘KAATSU’ Resistance Training.” International Journal of KAATSU Training Research, vol. 1, no. 1, 2005, pp. 6–12., doi:10.3806/ijktr.1.6.
Fatela, Pedro, et al. “Acute Effects of Exercise under Different Levels of Blood-Flow Restriction on Muscle Activation and Fatigue.” European Journal of Applied Physiology, vol. 116, no. 5, 2016, pp. 985–995., doi:10.1007/s00421-016-3359-1.
Glover, Elisa I., et al. “Immobilization Induces Anabolic Resistance in Human Myofibrillar Protein Synthesis with Low and High Dose Amino Acid Infusion.” The Journal of Physiology, vol. 586, no. 24, 2008, pp. 6049–6061., doi:10.1113/jphysiol.2008.160333.
Hughes, Luke, et al. “Blood Flow Restriction Training in Clinical Musculoskeletal Rehabilitation: a Systematic Review and Meta-Analysis.” British Journal of Sports Medicine, vol. 51, no. 13, 2017, pp. 1003–1011., doi:10.1136/bjsports-2016-097071.
Jessee, Matthew B., et al. “Mechanisms of Blood Flow Restriction.” Techniques in Orthopaedics, vol. 33, no. 2, 2018, pp. 72–79., doi:10.1097/bto.0000000000000252.
Kraemer, WJ, et al. “Progression Models in Resistance Training for Healthy Adults.” Medicine & Science in Sports & Exercise, vol. 41, no. 3, 2002, pp. 687–708., doi:10.1249/mss.0b013e3181915670.
Laurentino, Gilberto Candido, et al. “Strength Training with Blood Flow Restriction Diminishes Myostatin Gene Expression.” Medicine & Science in Sports & Exercise, vol. 44, no. 3, 2012, pp. 406–412., doi:10.1249/mss.0b013e318233b4bc.
Loenneke, Jeremy, et al. “The Acute Muscle Swelling Effects of Blood Flow Restriction.” Acta Physiologica Hungarica, vol. 99, no. 4, 2012, pp. 400–410., doi:10.1556/aphysiol.99.2012.4.4.
Mattocks, Kevin T., et al. “The Application of Blood Flow Restriction.” Current Sports Medicine Reports, vol. 17, no. 4, 2018, pp. 129–134., doi:10.1249/jsr.0000000000000473.
Nakajima, T., et al. “Use and Safety of KAATSU Training:Results of a National Survey.” International Journal of KAATSU Training Research, vol. 2, no. 1, 2006, pp. 5–13., doi:10.3806/ijktr.2.5.
Nielsen, Jakob Lindberg, et al. “Proliferation of Myogenic Stem Cells in Human Skeletal Muscle in Response to Low-Load Resistance Training with Blood Flow Restriction.” The Journal of Physiology, vol. 590, no. 17, 2012, pp. 4351–4361., doi:10.1113/jphysiol.2012.237008.
Ohta, Haruyasu, et al. “Low-Load Resistance Muscular Training with Moderate Restriction of Blood Flow after Anterior Cruciate Ligament Reconstruction.” Acta Orthopaedica Scandinavica, vol. 74, no. 1, 2003, pp. 62–68., doi:10.1080/00016470310013680.
Pierce, Joseph R., et al. “Growth Hormone and Muscle Function Responses to Skeletal Muscle Ischemia.” Journal of Applied Physiology, vol. 101, no. 6, 2006, pp. 1588–1595., doi:10.1152/japplphysiol.00585.2006.
Pope, Zachary K., et al. “Exercise and Blood Flow Restriction.” Journal of Strength and Conditioning Research, vol. 27, no. 10, 2013, pp. 2914–2926., doi:10.1519/jsc.0b013e3182874721.
Schoenfeld, Brad J. “Potential Mechanisms for a Role of Metabolic Stress in Hypertrophic Adaptations to Resistance Training.” Sports Medicine, vol. 43, no. 3, 2013, pp. 179–194., doi:10.1007/s40279-013-0017-1.
Schoenfeld, Brad J. “The Mechanisms of Muscle Hypertrophy and Their Application to Resistance Training.” Journal of Strength and Conditioning Research, vol. 24, no. 10, 2010, pp. 2857–2872., doi:10.1519/jsc.0b013e3181e840f3.
Schoenfeld, Brad Jon, and Alan Albert Aragon. “How Much Protein Can the Body Use in a Single Meal for Muscle-Building? Implications for Daily Protein Distribution.” Journal of the International Society of Sports Nutrition, vol. 15, no. 1, 2018, doi:10.1186/s12970-018-0215-1.
Slysz, Joshua, et al. “The Efficacy of Blood Flow Restricted Exercise: A Systematic Review & Meta-Analysis.” Journal of Science and Medicine in Sport, vol. 19, no. 8, 2015, pp. 669–675., doi:10.1016/j.jsams.2015.09.005.
Takarada, Yudai, et al. “Rapid Increase in Plasma Growth Hormone after Low-Intensity Resistance Exercise with Vascular Occlusion.” Journal of Applied Physiology, vol. 88, no. 1, 2000, pp. 61–65., doi:10.1152/jappl.2000.88.1.61.
Wall, Benjamin T., et al. “Disuse Impairs the Muscle Protein Synthetic Response to Protein Ingestion in Healthy Men.” The Journal of Clinical Endocrinology & Metabolism, vol. 98, no. 12, 2013, pp. 4872–4881., doi:10.1210/jc.2013-2098.
Wilson, Jacob M., et al. “Practical Blood Flow Restriction Training Increases Acute Determinants of Hypertrophy Without Increasing Indices of Muscle Damage.” Journal of Strength and Conditioning Research, vol. 27, no. 11, 2013, pp. 3068–3075., doi:10.1519/jsc.0b013e31828a1ffa.
Yasuda, Tomohiro, et al. “Muscle Activation during Low-Intensity Muscle Contractions with Restricted Blood Flow.” Journal of Sports Sciences, vol. 27, no. 5, 2009, pp. 479–489., doi:10.1080/02640410802626567.
